Gallbladder GuideUpdated 22 days ago
Gallbladder Guide
Many people, including healthcare professionals, often underestimate the gallbladder's significance. In the U.S., nearly 800,000 gallbladder removal surgeries occur annually due to gallstones, making it the most prevalent gastrointestinal issue leading to hospitalization. This contributes to $6 billion spent yearly on gallstone-related treatments! Gallbladder Guide If any of these sound familiar, your gallbladder may be trying to tell you it needs a little help! Gallbladder surgery, while necessary in emergency situations, does not address the underlying reasons why the gallbladder failed to perform. Gallbladder dysfunction isn't just limited to the gallbladder itself. Various conditions, linked to metabolic syndrome and digestive issues, affect gallbladder function.
Do I Have Gallbladder Dysfunction? Gallbladder symptoms start in the digestive system. It may not be dominant enough for you to notice at first. After some time, symptoms extend to other areas of the body. You may experience fatigue or get sick more often. Your appetite may be less, and your shoulders get tight. This may all be related to poor gallbladder function, but it’s hard to make the connection at first.
Common symptoms that point to gallbladder issues:
• Intolerance to fatty foods • Constipation • SIBO (small intestinal bacterial overgrowth) • Weight gain, metabolic syndrome • Pain in the upper right quadrant of your abdomen • Intolerance to high oxalate foods • Unexplained anemia • Bloating after meals • Full body itching • Right shoulder tightness • Nausea when eating fatty foods • Hormonal imbalances • Getting sick easily • Pain between the shoulder blades • Histamine intolerance • Mineral deficiencies • Deficiencies in vitamins A, D, E, and K • Grey to white colored stools • Bile reflux (acts like acid reflux) 9 • Yellowish skin and eyes Many people, including healthcare professionals, often underestimate the gallbladder's significance. In the U.S., nearly 800,000 gallbladder removal surgeries occur annually due to gallstones, making it the most prevalent gastrointestinal issue leading to hospitalization. This contributes to $6 billion spent yearly on gallstone-related treatments! Gallbladder Guide If any of these sound familiar, your gallbladder may be trying to tell you it needs a little help!
What Does Your Gallbladder Do?
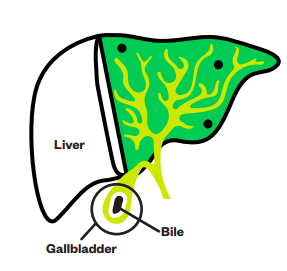
The gallbladder is a small storage pouch located below the liver. Its main job is to hold bile, a greenish digestive liquid produced by the liver. Your gallbladder springs into action when you enjoy foods loaded with fats like butter, nuts, eggs, and oils. When fats pass into the first part of the small intestine, the gallbladder releases bile into your small intestine. Bile breaks down these fats into smaller pieces so your body can absorb them. This process ensures you can get the nutrients you need from your diet! Fats are important for keeping your body in top shape—they help repair cells, give you lasting energy, and make hormones. Plus, fats are needed to absorb key vitamins like A, D, E, and K.
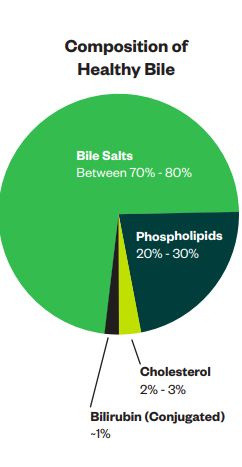
What is the Composition of Healthy Bile?
Water Makes up about 97-98% of bile and acts as the liquid base that dissolves the other ingredients. Being hydrated is essential.
Bile Salts Produced from cholesterol in the liver, combined with amino acids, primarily glycine and taurine. Bile salts are the primary driver of bile flowing from the liver into the gallbladder and out into the small intestine.
Phospholipids (phosphatidylcholine) Fats that are essential in transporting fat out of the liver. Additionally, they aid in bile being slippery and moving out of the gallbladder when needed.
Bilirubin A product of the breakdown of red blood cells.
Electrolytes Sodium and potassium keep bile slightly alkaline with a pH between 7 and 8. This alkalinity is crucial because bile neutralizes stomach acid as it moves into the small intestine. Electrolytes also support sufficient water moving into the bile, allowing bile to flow out of the gallbladder.
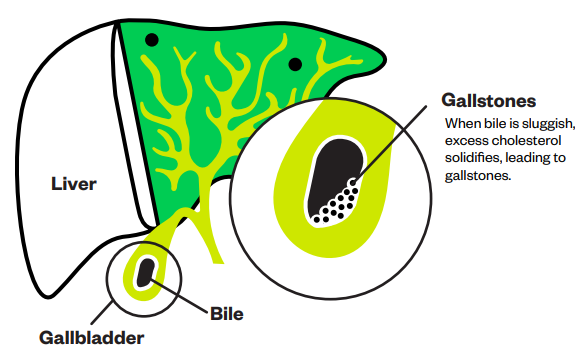
What Causes Gallstones to Form? For bile to stay fluid and prevent gallstone formation, there must be a proper balance between cholesterol and phosphatidylcholine, ideally at a 1:10 ratio. Typical bile solids consist of around 80% bile salts.16 Cholesterol is converted into bile salts in the liver. When the proportion of bile salts and/or phospholipids decreases and cholesterol levels remain too high, the bile thickens, making it sluggish. This happens because excess cholesterol solidifies, leading to gallstones.4 These gallstones block the bile ducts, stopping bile from reaching the small intestine. Over 70-85% of gallstones are predominantly cholesterol.11 Gallstones are significantly more common in women than in men. This is because estrogen increases cholesterol production while reducing bile acid synthesis.11 The PEMT enzyme is responsible for synthesizing phosphatidylcholine necessary to transport cholesterol out of the liver. Once removed from the liver, cholesterol is packaged into bile, thereby maintaining healthy cholesterol levels. When PEMT slows down or is impaired, cholesterol accumulates in the liver, leading to various health issues, including an increased risk of gallstone formation.11 Pregnant women are particularly vulnerable to gallstone formation due to several physiological changes.12 One major factor is choline deficiency. Over 90% of pregnant women are deficient in choline, a nutrient crucial for maintaining PEMT enzyme function and phosphatidylcholine production.13 A dirty PEMT, and low choline, contribute to higher cholesterol in the liver, and more sluggish bile, thus, the increased risk for gallstones.
Common reasons for an imbalanced ratio between phosphatidylcholine and cholesterol include:
• Fasting • Overeating • High-fat diet • Ketogenic diet • Vegan diets • Protein deficiency • Low dietary choline intake • Low dietary glycine intake • Methylation dysregulation • Dirty MTHFR • Dirty PEMT • Dehydration • Low stomach acid • Ongoing intake of proton pump inhibitors (PPIs) • Bacterial overgrowth of specific bacteria such as certain Clostridia species
You need optimal methylation, a clean MTHFR gene, a clean PEMT gene, and plenty of choline to make phosphatidylcholine. You also need amino acids (protein), especially glycine and taurine, for bile salt formation.
What Happens When You Don’t Have Healthy Bile Composition or Bile Flow?
Bile salts act like a ‘detergent’ to emulsify dietary fats and absorb fat-soluble nutrients. If you don’t have healthy bile composition or bile flow, you may end up with:
• Vitamin D and K deficiencies which may affect bone health • Vitamin D and A deficiencies which may affect immune health • Vitamin E deficiency and lower antioxidants • Increased dietary oxalate absorption, which may cause mineral deficiencies such as zinc, magnesium, and iron14 • Deficiencies in these minerals have their own set of consequences • Constipation • Fatty liver • High cholesterol • Sleep issues • Poor detoxification • Symptoms of excess estrogen such as PMS, PCOS, or endometriosis • SIBO3,6 • Acid reflux that doesn’t improve with antacids is typically bile reflux • Increased risk of gallstones
Bile salts help draw in water, making bile more fluid. When there aren’t enough bile salts, the body uses other substances like glutathione and bicarbonate to keep things moving smoothly independent of bile salts.15 This means your body might need more of these nutrients to help with digestion.
Gallbladder Dysfunction Increases SIBO Risk
The small intestine is typically not home to many microbes.6 Most of your gut bacteria reside in the large intestine, where they help break down food through fermentation. Stomach acid, along with bile, plays a protective role in this process. Stomach acid and bile eliminate microbes that are either sensitive to acid or high alkalinity, ensuring that unwanted bacteria do not thrive in the small intestine.
Bile affects small intestinal bacterial population in a few ways:
• Bile delivers IgA antibodies (part of your immune system) to the small intestine when it is released from the gallbladder.3,4 This keeps bacterial numbers under control. • Conjugated bile acids (bound to glycine or taurine) reduce bacteria's ability to move and spread to other tissues, such as lymph nodes. • Bile acids can ‘digest’ phospholipids and proteins that form part of bacterial cell walls. This creates holes in the walls of bacterial membranes, which causes them to ‘bleed out,’ shrink, and die.4 • Bile acids trigger the release of antimicrobial substances to help fight off harmful bacteria.1,3 This action occurs right at the junction of your small and large intestines, behind a gate known as the ileocecal valve. This gate prevents bacteria from moving back into the small intestine, maintaining a balanced gut environment and promoting digestive health.6 Bile is key to keeping your gut healthy by helping to prevent SIBO . While antibiotics or natural antimicrobials can knock it out, it's also essential to tackle any gallbladder issues. If your gallbladder isn't working properly, SIBO will make an unwelcome comeback.†
But here is the kicker! Bile-sensitive bacteria in the small intestine need a certain amount of bile to kill, similar to antibiotics. However, if you only take half your antibiotic course or consume meat that contains traces of antibiotics, you can make bacteria more antibiotic-resistant. The same happens with bile. If you only have small amounts of healthy bile released from the gallbladder, bile-sensitive bacteria may become more resistant and harder to kill. This is often the case when the gallbladder has been removed since no sac is left to store bile. Instead, bile gets produced by the liver and drip-feeds into the small intestine in small amounts. If you don’t produce enough bile to help digest fats from meals, you may struggle with loose stools. Additionally, if there is not enough to kill bile-sensitive bacteria in the small intestine, you may struggle with SIBO.
Poor Gallbladder Function Affects Hormone Detoxification
If you experience PMS or other symptoms of estrogen dominance, your gallbladder may need some attention for two key reasons: • Excess estrogen increases cholesterol synthesis and reduces bile acid production. This affects bile composition negatively and interferes with healthy gallbladder function.11 • The gallbladder itself plays an important role in estrogen detoxification in several ways. One key function is binding excess estrogen to bile acids for excretion. However, this estrogen detoxification is often badly disrupted by dysbiotic intestinal bacteria. Certain intestinal bacteria produce an enzyme called beta-glucuronidase. Beta-glucuronidase unbinds estrogen that is ready for excretion from bile acids. This allows estrogen to be reabsorbed back into the blood from the intestines. When beta-glucuronidase producing bacteria are allowed to overgrow it leads to elevated estrogen levels, contributing to estrogen dominance in both men and women. Additionally, bile acids released by the gallbladder activate receptors in the gut called ‘bile acid-activated nuclear receptors.1 When these receptors are activated by bile acids, they turn on metabolic pathways involved in reducing inflammation, metabolism, and detoxification, including the detoxification of estrogen5 to keep estrogen balanced. These bile acid sensitive receptors also suppress the overgrowth of the gut bacteria that produce the beta-glucuronidase enzyme. By doing this, estrogen doesn’t get reabsorbed and, thus, lowers estrogen.6 Supporting gallbladder function promotes better estrogen clearance, which helps alleviate symptoms of estrogen dominance. Healthy estrogen levels, on the other hand, support better bile composition and, thus, gallbladder function. They both need each other to maintain balance.
Poor Gallbladder Function Increases Oxalate Absorption
Humans cannot metabolize oxalates as we don’t have the enzymes oxalate oxidase or oxalate decarboxylase needed to break down oxalates. Many microorganisms, including certain gut bacteria, have these enzymes and can break down oxalates. If gut bacteria do not break down oxalates, they are typically excreted in the stool out of the gut. This requires healthy gallbladder function. Foods and drinks are considered high in oxalates if they contain more than 100 mg per serving. Very high is 300 mg or more. High amounts of oxalates are found in:
Food and Drink: • Raw spinach: 543 mg per cup • Cooked spinach: 755 mg per ½ cup • Beets: 152 mg per cup • Navy beans: 76 mg per cup • Firm tofu: 235 mg in 3 oz • Soy milk or soy yogurt: 336 mg per cup • Textured soy protein: 638 mg per 85 grams serving • Raspberries: 48 mg per cup • Dates: 24 mg each • Almond milk: 27 mg per cup • Black tea
When oxalates are absorbed from the gut into the bloodstream, they can cause problems such as kidney stones, joint pain, and bladder pain.
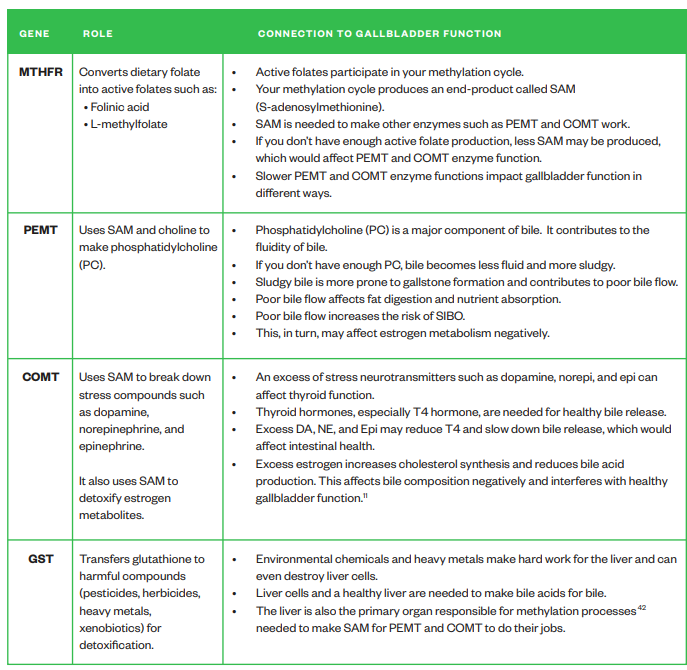
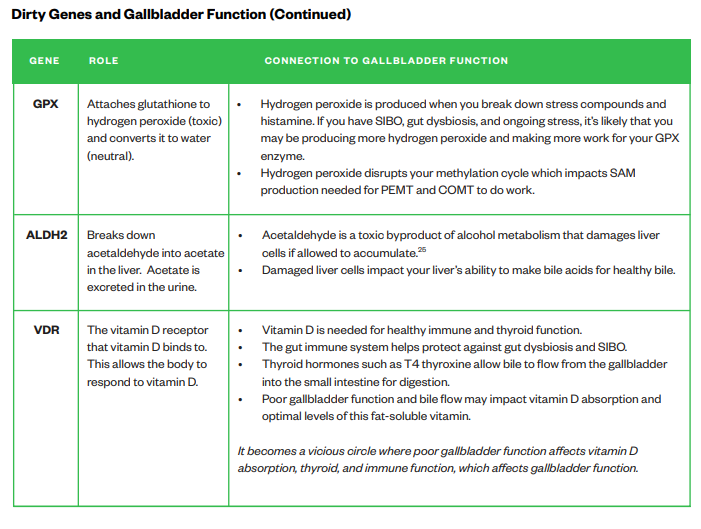
Dirty Genes and Gallbladder Function
Dirty Genes are genes that may cause slower enzyme function than typical, potentially causing health issues. This leads to health issues. You can inherit dirty genes at birth, or enzymes can become dirty due to factors like lifestyle choices, nutrient deficiencies, and environmental influences.
The chart on the following page depicts which enzymes, when dirty, contribute to gallbladder symptoms:
Stop Doing List
Don’t eat too many fatty foods such as butter, oils, animal fats, mayonnaise, canned fish in oil, and salad dressings if your gallbladder is struggling, at least temporarily. Eating high-fat foods makes more work for your gallbladder. If not enough bile is released fats will remain undigested which can cause digestive symptoms such as nausea, and at worst gallbladder attacks. It may also result in more oxalate absorption.22 Avoiding fats is not a long-term option. You need all types of fats, apart from transfats, to be healthy. The long-term option is to make sure your gallbladder functions as it should. Avoid deep-fried fast foods such as fries, fried chicken, or crumbed fish and seafood. This is always a good idea, but especially so if your gallbladder needs a break. Certain medications, such as PPIs (proton pump inhibitors) or antacids used for reflux reduce stomach acid production. This leads to less bile release when food enters the small intestine. Long-term use affects digestion and has flow-on effects further down the digestive tract such as increased risk of SIBO.23 Cholestyramine is a medication commonly used to lower cholesterol levels in the blood or to treat mold biotoxin illness. It grabs onto bile acids and stops them from being reabsorbed in the small intestine. Instead, you poop them out. Long-term use shrinks the bile acid pool and you have to make more from cholesterol.28 This requires more resources such as taurine and glycine. Do not stop any medications without consulting your prescribing healthcare practitioner.
Start Doing List
Eat more choline-rich foods as you need choline to make phosphatidylcholine for optimal bile production. These include egg yolks, liver, beef, chicken, and fish. Plant-based foods high in choline include soy, shiitake mushrooms, and broccoli. Eat more taurine-rich foods as you need taurine to make bile acids. This is typically not an issue as animal protein is high in taurine and our body can make some. However the majority of taurine our body needs is from dietary sources. Vegans may need to supplement with taurine as plant foods do not contain taurine. Seaweed contains some taurine but not a lot.25 Eat more folate-rich foods to help your MTHFR enzyme support your PEMT enzyme function and healthy bile production. These include eggs, green leafy vegetables (kale, broccoli, bok choy, dark-coloured lettuce), brussels sprouts, asparagus, legumes (beans, peas, chickpeas, lentils), tofu, and liver. Spinach is high in folate, but also high in oxalates, which is why we don’t recommend it as a good source of folate.29 Choose lean meats whilst you work on improving your gallbladder function. Cut off fat that you can see. Eat chicken or other poultry without the skin. Bake, broil, or grill meat instead of frying them in oil if your gallbladder needs a break. Eat grilled or baked fish instead of crumbed and deep-fried. Address SIBO if relevant. Work with a healthcare practitioner that can help you with treatment options. Bacteria overgrowing in the small intestine can migrate to the bile duct, causing inflammation and gallbladder and liver dysfunction.26 They can also change bile acids and convert them into more toxic bile acids that disrupt healthy digestive function.
Seeking Health’s Gallbladder Support Supplements
Seeking Health offers a range of gallbladder support supplements that support healthy bile formation and gallbladder function, formulated by epigenetics expert Dr. Ben Lynch, ND.† Consider starting with Bile Nutrients. This supplement supports healthy bile production and bile flow.† For the first 3 days, take 2 capsules before dinner. Then, take 4 capsules in divided serving sizes before lunch and before dinner. Some people do best when taking all 4 capsules before dinner. Experiment and see what works best for you.
If you’ve been neglecting your gallbladder for some time or it needs significant support, you may need to approach it more aggressively. Dr. Lynch formulated the Gallbladder and Bile Bundle making it easier for you, and 20% savings. The bundle consists of 4 supplements and a free copy of Dirty Genes:
Bile Nutrients A synergistic blend that contains taurine and glycine for bile acid conjugation and herbs that support healthy liver function, gallbladder stimulation, bile production, and digestion. For the first 3 days, take 2 capsules before dinner. Then, take 4 capsules in divided serving sizes before lunch and dinner. Bile Nutrients is vegan-friendly.†
Liver Nutrients Bile acids are made in the liver. Healthy gallbladder function needs healthy liver function. Take 1 capsule before or after dinner.†
Optimal Electrolyte Water makes up 95% of bile. If bile is dehydrated, then it’s sluggish and contributes to gallstones. Drink 1 serving upon waking and another 1 to 2 servings throughout the day as needed.
Ox Bile If you’ve had your gallbladder removed, have a very sluggish gallbladder, or suffer from SIBO, Ox Bile may be supportive. It will support your body’s balanced bile demand when needed and microbial balance in the small intestine. Take 1 capsule with every meal that contains fatty foods. Additionally, take 1 capsule on an empty stomach before bed to support healthy small intestine microbiome levels. As the name suggests, Ox Bile is not vegan-friendly.†
Additional support for your liver and gallbladder may be needed. Here are some additional recommendations for you to consider. Read through each one and see if they resonate with you:
Digestive Enzymes Helps support the breakdown of fats, proteins, carbohydrates, and smaller carbohydrates called disaccharides. Undigested food in the small intestine may serve as food for bacteria and yeasts in the small intestine and worsen SIBO. Take 1-2 capsules just before eating a meal.†
Vitamin D3 +K2 These fat-soluble vitamins are needed for healthy joints and bones. These nutrients may become deficient if gallbladder function is sub par and may need to be supplemented until gallbladder function is restored. Your healthcare practitioner can get your vitamin D levels tested. Take 1 capsule a day with food if needed.†
Can I take Bile Nutrients even if I don’t have a gallbladder? Yes! Your gallbladder was removed because you were likely not producing sufficient healthy bile in the first place. This led to your bile flow being too sluggish, which then led to cholesterol-based gallstones. Ultimately, this caused pain, and eventually, you had to get your gallbladder removed. While the removal of your gallbladder alleviated your pain and discomfort, it did absolutely nothing to improve the production of bile and the flow of your bile. The underlying issues of insufficient bile production and thick or insufficient bile flow are likely still present. Bile Nutrients supports healthy bile production and flow, which undoubtedly was an issue before the gallbladder was removed.†
I still have my gallbladder but have a history of gallstones. What should I take? Optimal PC, Bile Nutrients, Optimal Electrolyte, and Liver Nutrients may be good options for you. They will support healthy bile formation and release.†
I still have my gallbladder and have gallstones. What can I take? Optimal PC, Optimal Electrolyte, Liver Nutrients, and Ox Bile may be good options for you. Do not take Bile Nutrients without checking with your healthcare practitioner first.†
I still have my gallbladder and have gallstones. I’m in pain. What can I take? If you are too uncomfortable, go see your healthcare practitioner. Some suggestions in the meantime include: • Warm soups that are not fatty, like a vegetable soup. • 100% organic beet juice from the grocery store. • Taking a TUDCA supplement with each meal. TUDCA is a secondary bile acid that helps to support healthy bile flow, which can be beneficial for those concerned about gallstones. 17 • Eating smaller meals. • Not overeating. • Avoiding fats, oils, nuts, and seeds. • Taking Digestive Enzymes (1 - 2 capsules) with each meal to support healthy digestion.† • Applying a castor oil pack over your entire abdomen, being sure to cover your gallbladder area.
Do I have to take Bile Nutrients or Ox Bile with every meal? Not necessarily. If you’re simply having fruit for breakfast, you don’t need to take supplements that stimulate bile production because you’re not eating fat. Use these supplements when you consume meals that contain fat, even if it’s healthy fat.† 1 4 †These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
I’m pregnant. Can I use Bile Nutrients? If you are pregnant, you cannot use Bile Nutrients because they contain herbs. We generally don't suggest herbal products during pregnancy unless specified by your primary health practitioner. Consider using Optimal PC instead. Take 1 capsule of Optimal PC with dinner each evening to support a healthy gallbladder, bile production, and flow.† The demand for phosphatidylcholine increases during pregnancy, which is a key reason why many women end up with gallbladder-related symptoms post-pregnancy. I’m taking Bile Nutrients and feeling more constipated. Is this normal? Some people notice a worsening of constipation at first when taking Bile Nutrients. If this happens, simply drink a glass of Optimal Electrolyte, and increase the amount of Bile Nutrients you take. If you are just taking 2 capsules before dinner, take 2 before lunch. If you already are taking 2 and 2, consider switching to 4 capsules all at once before dinner.
I’m following a carnivore diet. Should I take Ox Bile? You can use Ox Bile or Bile Nutrients when consuming fatty meats. You may want to consider taking Digestive Enzymes as it’s more comprehensive and supports the healthy digestion of protein and fats.†
I’m using Ox Bile to support my SIBO treatment plan and taking it with my probiotics at bedtime. Can I take these together?† Ideally not. There may be some species in your probiotics that are bile acid-sensitive. Take Ox Bile before bed on an empty stomach and take your probiotics in the morning with breakfast.
I’m taking Ox Bile, Bile Nutrients, and Optimal PC and getting diarrhea. Is this normal? You are most likely taking too many gallbladder supplements. Remember that bile is your body’s natural laxative. Cut out the Ox Bile and see how you go with just Bile Nutrients and Optimal PC. If you’re still experiencing diarrhea, cut out Bile Nutrients. If still experiencing loose stools, consider 1 capsule of ProBiota HistaminX and 1 capsule of Saccharomyces Boulardii after dinner. Adding bulk to your stool may be helpful. Consider taking 3 to 5 capsules of Gut Nutrients before bed on an empty stomach—or any time of day as long as it’s away from food by about 1 hour. If diarrhea persists, check in with your healthcare provider.
I have hypothyroidism. Could this be contributing to my constipation and gallbladder function? Yes. Thyroxine (T4 thyroid hormone) is necessary to help the Sphincter of Oddi to relax and support the MTHFR enzyme. The Sphincter of Oddi regulates bile release from the gallbladder into the small intestine.18 If thyroxine is deficient, less bile may be released into the small intestine, contributing to SIBO and/or constipation. If you have low or low-normal thyroxine levels, consider supplementing with iodine.† 1 5 †These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
I have an overgrowth of gut bacteria (such as Bilophila) that consume bile acids. Can I take gallbladder supplements? This is an interesting question, and you will likely get different answers from experts. Many believe they should avoid taurine, TUDCA, gallbladder supplements, and ox bile. Certain gut organisms consume bile acids. At the same time, this may result in an imbalance of bile acids in the gut and liver and/or gallbladder dysfunction (since bile acids must be recycled). It is also common to see higher levels of taurine excretion during gut infections, which may cause taurine deficiencies. Taurine is important for magnesium absorption.† We recommend that Liver Nutrients, Bile Nutrients, and Optimal PC are OK and possibly needed to support gallbladder health.† Always check in with your healthcare provider when considering adding new supplements to your routine. The key here may be to look at your microbial diversity in the gut. If you have undergrowth of healthy species such as Faecalibacterium prausnitzii, Akkermansia, Roseburia, Coprococcus, Bifido- and Lactobacilli species, then focus on growing these instead as opposed to avoiding gallbladder support. Saccharomyces Boulardii supports a healthy level of Faecalibacterium prausnitzii, while ProBiota HistaminX supports a healthy level of both Bifido and Lacto species.†
I’m quite sensitive to supplements. Can I open Ox Bile capsules and use a lower dose? Yes, you may. It will not taste very good because it is bitter. You may want to mix it with some food, such as gluten-free bread, and roll it up in a ball before swallowing it with some filtered water.
Where is Ox Bile sourced from? Seeking Health Ox Bile is from a bovine source, free-range oxen, with no usage of synthetic hormones or antibiotics.
Is Ox Bile vegetarian- or vegan-friendly? No. It is an animal-based product and is not considered vegetarian- or vegan-friendly. Use Bile Nutrients instead.
Is Ox Bile acid-resistant? Ox Bile does not need to be in acid-resistant capsules as it survives the stomach acid.†
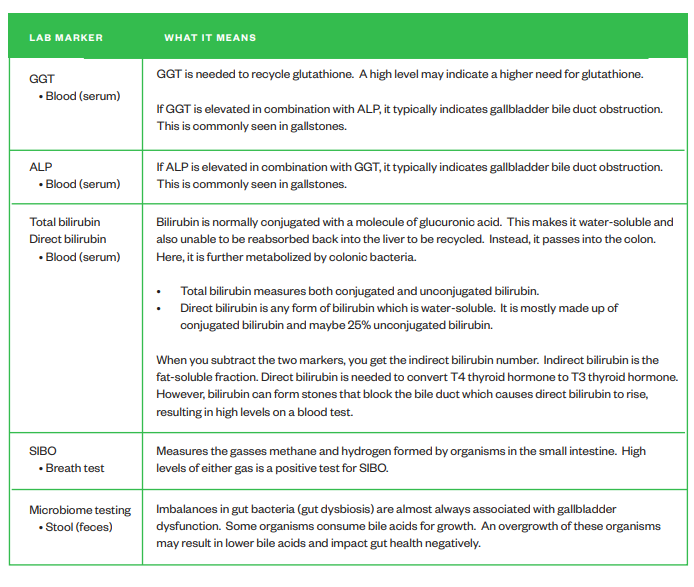
Lab Testing Lab testing is often used to see if your gallbladder needs some support.
Common lab tests and markers include: • GGT (serum) - high • ALP (serum) - high • Bilirubin (serum) - high • SIBO (breath) - positive • Microbiome (stool) - positive for gut dysbiosis